This information is for healthcare professionals based in EU countries only.
Are you a healthcare professional?
Patients with FCS have plasma triglyceride (TG) levels ranging from 10 to 100 times the normal value.1* Chylomicrons are formed in the intestines and transport TGs from the intestines to the rest of the body.5
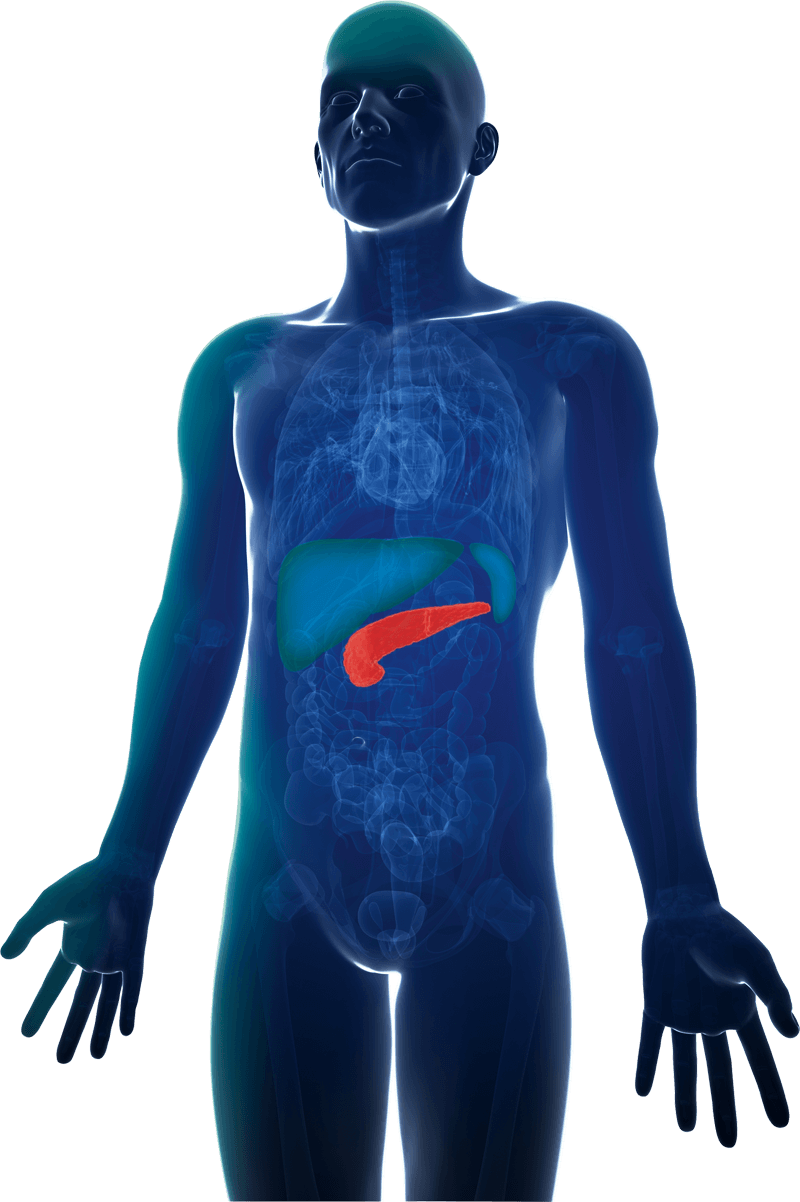
FCS is a rare autosomal recessive disease associated with limited functionality of the enzyme lipoprotein lipase (LPL), resulting in accumulation of TG in the blood. The acculmulation of chylomicrons leads to different symptoms and complications. The most severe complication is increased risk of recurrent and potentially fatal acute pancreatitis.1,6
Patients affected by chylomicronemia due to LPL deficiency are at much greater risk of pancreatitis than those with hypertriglyceridemia caused by other conditions, suggesting a direct correlation between accumulation of chylomicrons and pancreatitis.6
FCS affecting daily living
Patients with FCS frequently experience manifestations that have a considerable impact on their daily lives. 75% of patients felt that FCS negatively impacted their social relationships.2
*Normal TG value 17-170 mmol/L
Fatigue
Forgetfulness
Lipaemia retinalis
Vomiting or diarrhoea
Neurological symptoms
such as memory loss and feeling depressed
Frequent abdominal and back pain
Numbness or tingling of digits
Hepatosplenomegaly
Pancreatitisa
Xanthoma2-4
Due to its rarity, the recognition and correct diagnosis of FCS is challenging.6 Around 67% of patients have described being misdiagnosed.2

Normal
blood sample
Lipemic
blood sample
Clinical characteristics to look out for7
FCS score
A panel of European experts have provided guidance on the diagnostic strategy surrounding FCS and proposed an algorithm-based diagnosis score for identification of these patients, which can be readily translated into practice.7
FCS is associated with limited functionality of lipoprotein lipase (LPL). The loss of functionality in LPL makes the LPL-pathway inefficient and leads to accumulation of chylomicrons in the blood.
LPL pathway is the primary mechanism by which plasma triglycerides (TGs) are hydrolyzed leading to subsequent efficient removal. Apolipoprotein C-III (ApoC-III) modulates triglyceride levels primarily by inhibiting the LPL-dependent pathway but also the LPL-independent pathway.
Triglycerides enter the blood plasma from dietary fat absorption in the intestine, in the form of chylomicrons and from the liver in the form of very low density lipoprotein (VLDL) particles.
The loss of function mutations in LPL makes the LPL-pathway inefficient and leads to accumulation of chylomicrons in the blood.
This information is for healthcare professionals based in EU countries only.
Are you a healthcare professional?